Mental Status Examination Cheat Sheet: Your Ultimate Guide
Oct 4, 2024
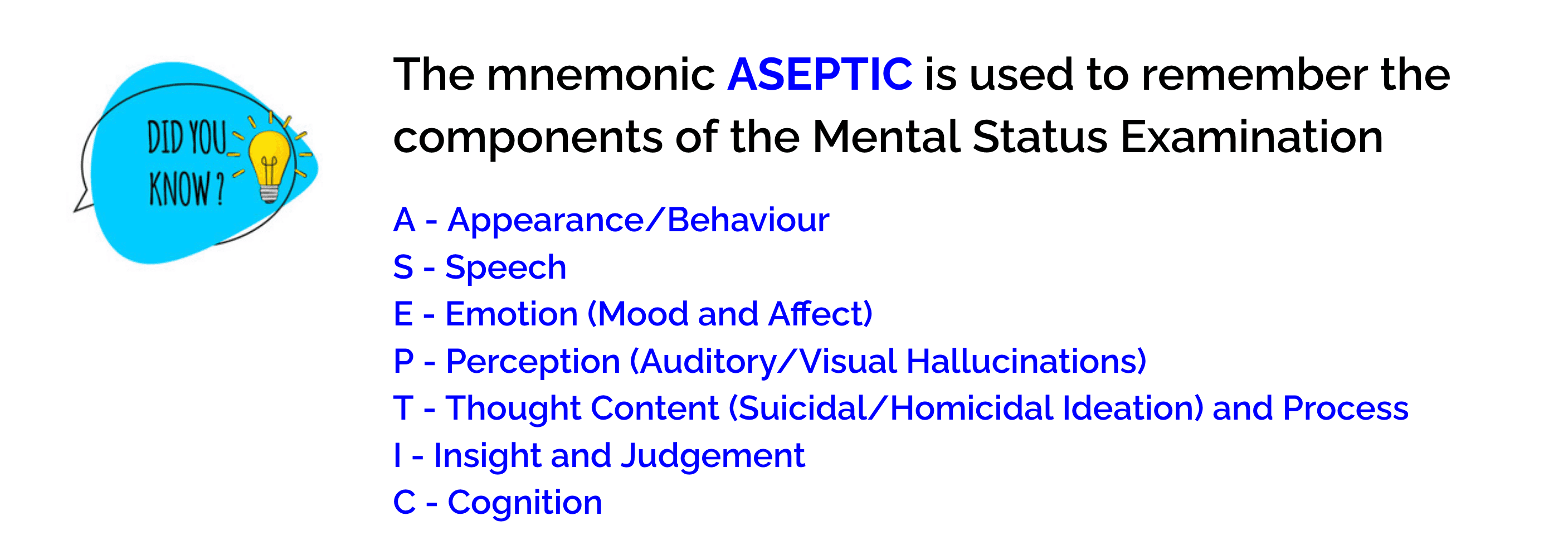
As a mental health professional, you know that conducting a thorough mental status examination is crucial to understanding your client's psychological state. This comprehensive assessment tool allows you to evaluate various aspects of a person's mental functioning, providing valuable insights for diagnosis and treatment planning. The mental status exam serves as a cornerstone of psychiatric evaluation and cognitive assessment, helping you gage everything from mood and affect to thought processes and content.
In this ultimate guide, you'll discover a practical mental status exam cheat sheet to streamline your assessment process. We'll break down the key components of the MSE, including general appearance and behavior, speech and language, mood and affect evaluation, thought analysis, and cognitive function assessment. You'll learn how to use MSE terms effectively, interpret mental status exam descriptors, and create a detailed MSE checklist. Whether you're looking for a mental status exam template PDF or seeking to enhance your understanding of MSE example PDFs, this guide will equip you with the knowledge and tools to conduct thorough and insightful mental health status examinations. (Well, if you actually need it in PDF format, just go File-Print-Save as PDF in your browser menu)
Understanding the Mental Status Examination
The mental status examination (MSE) is a crucial tool in psychiatric and neurological practice. It provides a comprehensive snapshot of a patient's mental state, helping clinicians make accurate diagnoses and develop effective treatment plans. This systematic assessment covers various aspects of mental functioning, from appearance and behavior to cognitive abilities and emotional state.
Purpose of MSE
The primary goal of the mental status exam is to get a detailed picture of a patient's current mental state. This information, combined with the patient's history, allows healthcare providers to:
• Identify symptoms and signs of mental disorders
• Assess potential risks to the patient or others
• Generate a psychiatric formulation
• Create a tailored treatment plan
The MSE is designed to capture both objective and subjective aspects of mental illness. It serves as a baseline for tracking changes in a patient's condition over time, which is essential for monitoring treatment progress.
When is it performed?
Mental status exams are conducted in various healthcare settings and situations:
• During initial psychiatric assessments in outpatient or hospital settings
• As part of regular check-ups or follow-up appointments
• When a change in mental status is suspected
• To evaluate improvement or deterioration in a patient's condition
Healthcare providers may perform parts of the MSE during routine visits to detect early signs of mental health or neurological conditions. The frequency of these exams can vary depending on the patient's needs and the healthcare setting.
Who conducts the exam?
To establish a medically determinable physical or mental impairment, the mental status exam must be performed by an "Acceptable Medical Source" (AMS) [1]. These professionals include:
• Physicians
• Psychologists
• Advanced Practice Nurse Practitioners (APRNs)
• Physician Assistants (PAs)
It's worth noting that the APRN category encompasses Certified Nurse Midwives, Nurse Practitioners, Certified Registered Nurse Anesthetists, and Clinical Nurse Specialists. Audiologists are also considered acceptable medical sources for hearing-related disorders.
While the MSE was historically associated with psychiatrists, it's now used across various medical specialties. Family medicine, emergency medicine, and internal medicine practitioners often incorporate elements of the mental status exam into their patient evaluations. The extent and depth of the examination may vary based on the clinician's expertise and the specific needs of the patient.
Remember, the mental status exam is just one piece of the puzzle. Healthcare providers consider it alongside other factors like the patient's medical history, physical exam results, and laboratory data to form a comprehensive understanding of the patient's condition. This holistic approach ensures that diagnoses are accurate and treatment plans are tailored to each individual's unique needs.
General Appearance and Behavior
When conducting a mental status examination, observing the patient's general appearance and behavior provides valuable insights into their psychological state. This section of the assessment focuses on three key areas: physical appearance, behavior and mannerisms, and attitude towards the examiner.
Observing physical appearance
The first step in evaluating general appearance involves noting the patient's physical characteristics. Pay attention to their build, comparing their apparent age to their actual age. This can offer clues about potential health issues or lifestyle factors. For instance, a patient who appears older than their stated age might be dealing with severe medical conditions or substance abuse problems [1].
Grooming and hygiene are crucial indicators of a person's functional level. Poor self-care might suggest underlying mental health issues, such as severe depression or schizophrenia [1]. However, it's essential to consider the patient's history and context when interpreting these observations.
Clothing choices can also be telling. Are the patient's clothes appropriate for the weather and circumstances? Excessively formal, flamboyant, or provocative attire might indicate certain mental states or conditions . Additionally, note any unusual objects the patient might be carrying, as these can provide further insights into their mental state.
Assessing behavior and mannerisms
Observing the patient's behavior during the interview is crucial. Pay attention to their level of distress, which could stem from underlying medical problems or acute symptoms. Note how they interact with you as the interviewer. Are they cooperative, agitated, avoidant, or unable to be redirected? These behaviors can offer clues about the patient's mental state and potential diagnoses [1].
Watch for psychomotor signs such as restlessness, fidgeting, or slowed movements. These can be indicators of various mental health conditions. Also, observe the patient's eye contact, posture, and gestures during the conversation. Abnormal movements or postures might suggest certain mental health issues or medication side effects .
It's important to remain objective when evaluating behavior. If there's a discrepancy between the patient's subjective report and your observations, maintain a neutral stance and consider all possible explanations.
Evaluating attitude towards examiner
The patient's attitude towards you as the examiner can provide valuable information about their mental state and potential diagnoses. Observe whether they appear relaxed and engaged or hostile and confrontational. Pay attention to the level of eye contact – is it reduced or inappropriately intense?
Building rapport with the patient is crucial for a productive examination. Note whether you're able to establish a positive connection or if there's tension or discomfort in the interaction. A positive rapport can aid in forming a constructive therapeutic relationship, while a negative one might hinder the assessment and treatment process .
Throughout the examination, remain alert to any signs that the patient might be responding to hallucinations or other stimuli not apparent to you. This could include unexplained actions, verbal outbursts, or apparent attention to unseen or unheard stimuli .
By carefully observing and documenting these aspects of general appearance and behavior, you'll gather crucial information to inform your overall mental status examination and guide your diagnostic process.
Speech and Language Assessment
Assessing speech and language is a crucial component of the mental status examination. This evaluation provides valuable insights into a patient's cognitive functioning, emotional state, and potential mental health conditions. By carefully observing various aspects of speech, you can gather important information to inform your overall assessment.
Rate and volume of speech
The rate and volume of speech can offer significant clues about a patient's mental state. Pay attention to how quickly or slowly the patient speaks, as well as the loudness or softness of their voice. For instance, slow speech (bradylalia) may indicate depression, Parkinson's disease, or cognitive impairment. On the other hand, rapid speech (tachylalia) could suggest mania, anxiety, or the use of stimulants.
Pressured speech, characterized by fast talking without breaks and an inability to be redirected, is often associated with mania or severe anxiety. The volume of speech can also be telling. Loud speech (hyperphonia) might be a personality trait or indicate hearing impairment or mania, while weak or soft speech (hypophonia) could suggest shyness, anxiety, depression, or Parkinson's disease.
Fluency and articulation
Observing the fluency and articulation of speech can reveal potential neurological or psychological issues. Take note of any stuttering, slurring, or hesitations in the patient's speech. Stuttering, which involves repetition, prolongation, or pauses in speech, may be developmental, neurogenic, or psychogenic in nature. Cluttering, characterized by rapid and disorganized speech with excessive word and phrase repetitions, is often related to language or learning disabilities.
Other factors that can affect fluency and articulation include dysphasia/aphasia, dysarthria, confusion (which may be due to delirium, dementia, or intellectual disability), hearing impairment, language barriers, or intoxication. Pay attention to the patient's ability to articulate words clearly and maintain a smooth flow of speech throughout the conversation.
Content and coherence
The content and coherence of speech provide crucial information about a patient's thought processes and potential mental health conditions. Assess whether the patient's speech is logical, organized, and relevant to the conversation. Look for signs of tangentiality, where the patient goes off on tangents and fails to return to the main point, or circumstantiality, where they provide excessive and unnecessary details before reaching the point.
Observe the patient's ability to maintain a coherent train of thought and whether their ideas flow logically from one to another. Incoherent or disorganized speech may indicate thought disorders associated with conditions such as schizophrenia. Pay attention to any unusual content, such as delusional beliefs or hallucinations, which may be revealed through the patient's speech.
By carefully assessing these aspects of speech and language during the mental status examination, you can gather valuable information to support your overall evaluation and guide your diagnostic process. Remember to consider the patient's cultural background, education level, and any language barriers that may influence their speech patterns.
Mood and Affect Evaluation
Assessing mood and affect is a crucial part of the mental status examination, providing valuable insights into a patient's emotional state and potential mental health conditions. To conduct a thorough evaluation, it's essential to understand the difference between mood and affect and how to assess each accurately.
Differentiating between mood and affect
Mood refers to the patient's internal, subjective emotional state, typically lasting for an extended period. It's one of the few elements of the mental status exam that relies on both patient self-report and physician observation. To assess mood, ask the patient to describe their feelings over the past few weeks, rather than just at the moment. You might also consider using a rating scale, asking the patient to rate their mood from 1 to 10 (with 1 being sad and 10 being happy) at each visit.
Affect, on the other hand, is the physician's objective observation of the patient's expressed emotional state. It's assessed through the patient's facial expressions, body language, tone of voice, and overall demeanor during the conversation. Unlike mood, affect can change rapidly and is often more immediate and observable.
Types of mood
When evaluating mood, consider using descriptors such as:
• Euthymic (normal)
• Depressed
• Anxious
• Irritable
• Euphoric
• Apathetic
It's important to note the patient's exact words when they describe their mood. Ask open-ended questions like, "How have you been feeling recently?" or "Have you felt irritable, angry, depressed, or unmotivated lately?" This approach allows for a more comprehensive understanding of the patient's emotional state.
Characteristics of affect
When assessing affect, pay attention to the following aspects:
Intensity: Observe the strength and depth of the patient's emotional expressions. Affect can range from normal to blunted or flat.
Range: Examine the variety of emotions displayed during the conversation. Affect can be described as broad, restricted, or constricted.
Stability: Note how consistently the patient's emotions change with the flow of the conversation. Affect may be stable or labile (rapidly fluctuating).
Appropriateness: Evaluate whether the patient's emotional expression matches the content of their speech. Incongruent affect might indicate certain mental health conditions.
Quality: Use descriptors such as sad, angry, hostile, indifferent, or anxious to characterize the patient's affect.
To get a comprehensive picture of the patient's affect, engage them in a wide-ranging conversation covering various topics, including personal losses, relationships, achievements, and experiences. Observe their emotional responses throughout the interaction.
Remember that affect may or may not be congruent with mood. For instance, a patient might report feeling "great" while displaying a tearful affect, indicating incongruence between mood and affect. This discrepancy can provide valuable information about the patient's emotional state and potential underlying mental health issues.
By carefully assessing both mood and affect during the mental status examination, you'll gather crucial information to support your overall evaluation and guide your diagnostic process. This comprehensive approach ensures a more accurate understanding of the patient's emotional well-being and helps inform appropriate treatment strategies.
Thought Process and Content Analysis
Assessing thought process and content is a crucial component of the mental status examination. This evaluation provides valuable insights into a patient's cognitive functioning and potential mental health conditions. By carefully observing various aspects of thought organization and content, you can gather important information to inform your overall assessment.
Assessing thought organization
When evaluating thought process, pay attention to how the patient organizes and expresses their ideas. A normal thought process is typically linear and goal-directed. However, you may encounter various irregular thought processes, such as:
• Circumstantial: The patient's thoughts are connected but go off-topic before returning to the original subject.
• Tangential: Thoughts go off-topic without returning to the original point.
• Flight of ideas: Similar to tangential thinking, but the connection between thoughts is less obvious and challenging to follow.
• Loose or disorganized: No clear connection between thoughts, making it difficult to follow. • Perseveration: The patient repeatedly returns to the same subject, regardless of the topic or question.
• Thought blocking: Interruptions in thoughts, making it challenging to start or finish a thought.
Identifying delusions and hallucinations
Delusions and hallucinations are key symptoms of psychosis that can significantly impact a patient's perception of reality. Delusions are fixed, false beliefs that persist despite evidence to the contrary. Common types of delusions include:
• Persecutory: Belief that others are trying to harm or spy on them.
• Grandiose: Exaggerated beliefs about one's importance, power, or identity.
• Somatic: False beliefs about one's body or health.
• Erotomanic: Belief that someone, often a celebrity, is in love with them.
Hallucinations, on the other hand, involve sensory perceptions without external stimuli. These can be:
• Auditory: Hearing voices or sounds that aren't there.
• Visual: Seeing things that don't exist.
• Tactile: Feeling sensations on the skin without a physical cause.
• Olfactory: Smelling odors that aren't present.
• Gustatory: Tasting flavors without consuming anything.
To identify these symptoms, ask open-ended questions and observe the patient's behavior throughout the interview. Be mindful that patients may be hesitant to disclose such experiences due to fear of judgment or persecution.
Evaluating suicidal/homicidal ideation
Assessing suicidal and homicidal ideation is a critical aspect of the mental status examination. When evaluating these thoughts, consider:
• Passive vs. active thoughts: Determine if the patient has passive wishes or active plans to harm themselves or others.
• Frequency and intensity of thoughts: Ask about how often these thoughts occur and how strong they are.
• Presence of a plan: Inquire if the patient has developed a specific plan to act on these thoughts.
• Access to means: Assess if the patient has access to methods to carry out their plan.
• Protective factors: Identify any reasons the patient has for living or not acting on these thoughts.
Remember to approach these topics with sensitivity and empathy, as patients may be reluctant to discuss such thoughts. If you identify significant risk, conduct a comprehensive suicide or violence risk assessment and take appropriate safety measures.
Cognitive Function Assessment
Assessing cognitive function is a crucial component of the mental status examination. This evaluation provides valuable insights into a patient's mental processing abilities and can help identify potential cognitive impairments. The assessment typically covers three main areas: orientation and attention, memory evaluation, and abstract thinking and judgment.
Orientation and attention
Orientation refers to a patient's awareness of time, place, and person. To evaluate orientation, you might ask questions like "What is today's date?" or "Where are we right now?" These simple queries can reveal a lot about a patient's cognitive state.
Attention is another critical aspect of cognitive function. It can be tested using various methods, such as asking the patient to spell a five-letter word backward or perform serial subtractions. For example, you might ask the patient to subtract 7 from 100 repeatedly [3]. The Connors Continuous Performance Test is a more comprehensive tool for assessing attention and concentration [4].
Memory evaluation
Memory assessment is a key part of the cognitive function evaluation. It's typically divided into short-term and long-term memory tests.
To test short-term memory, you might ask the patient to recall three objects after a few minutes. For long-term memory, you could ask about past events, such as "What color suit did you wear at your wedding?" [3]
It's important to note that memory is a complex domain. It includes procedural memory (for tasks like driving a car), declarative memory (for facts and events), and episodic memory (for specific experiences). When evaluating memory, it's crucial to document which aspects you're assessing [4].
Abstract thinking and judgment
Abstract thinking involves the ability to deal with concepts and ideas rather than concrete objects. It can be tested by asking patients to explain similarities between objects or interpret proverbs. For example, you might ask, "What's the similarity between an apple and a pear?" or "What does the proverb 'People who live in glass houses shouldn't throw stones' mean?" [3]
Judgment refers to a person's capacity to make good decisions and act on them. To assess judgment, you might present hypothetical situations and ask how the patient would respond. For instance, "What would you do if you found a stamped letter on the sidewalk?" [3]
It's worth noting that a patient's level of judgment may not always correlate with their level of insight into their condition. A patient might have poor insight into their illness but still demonstrate good judgment in everyday situations [3].
By thoroughly assessing these aspects of cognitive function, you can gain a comprehensive understanding of a patient's mental status. This information is invaluable for diagnosing conditions, tracking changes over time, and developing effective treatment plans.
Conclusion
The mental status examination stands as a cornerstone in psychiatric and neurological practice, offering a comprehensive snapshot of a patient's mental state. This guide has broken down the key components of the MSE, from assessing general appearance and behavior to evaluating cognitive function. By mastering these elements, healthcare professionals can gather crucial information to support their overall evaluation and guide their diagnostic process.
Ultimately, the mental status exam is more than just a checklist; it's a powerful tool to understand and help patients. It allows healthcare providers to identify symptoms, assess risks, and create tailored treatment plans. As you apply these insights in your practice, remember that each patient is unique. The MSE, combined with other clinical data, helps paint a complete picture of an individual's mental health, paving the way for more effective and personalized care.
References
[1] - https://my.clevelandclinic.org/health/diagnostics/mental-status-exam
[3] - https://www.merckmanuals.com/professional/neurologic-disorders/neurologic-examination/how-to-assess-mental-status
[4] - https://www.ncbi.nlm.nih.gov/books/NBK556049/
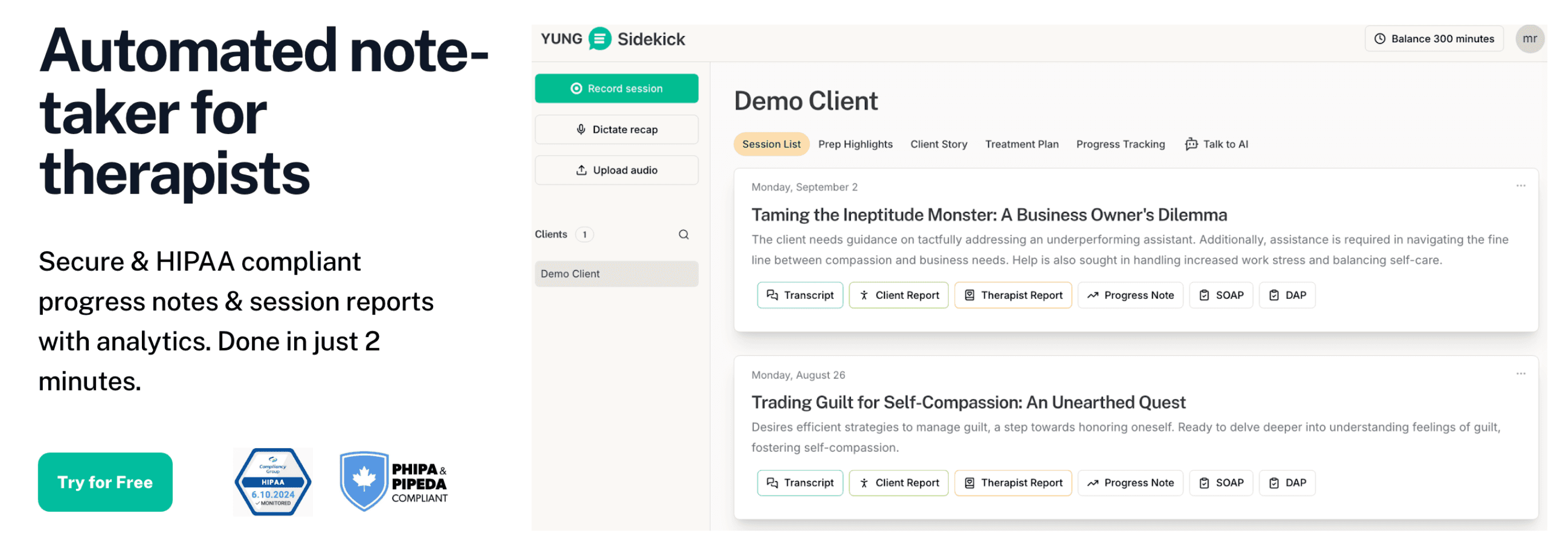
If you’re ready to spend less time on documentation and more on therapy, get started with a free trial today
Not medical advice. For informational use only.
Outline
More articles








